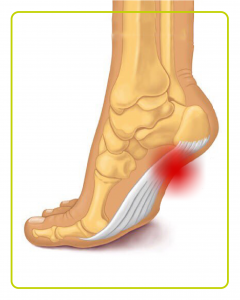
 Athletes, particularly runners, should always go through a thorough stretching program to properly warm-up the muscles. They should decrease the distance of their walk or run, apply ice after the activity and avoid any uphill climbs. They should use an orthotic device, heel cup, or heel cradle for extra support. A heel cup or heel cradle elevates the heel and hereby reduces stress and pressure on the achilles tendon. The device should be made with light-weight, shock absorbing materials.
Athletes, particularly runners, should always go through a thorough stretching program to properly warm-up the muscles. They should decrease the distance of their walk or run, apply ice after the activity and avoid any uphill climbs. They should use an orthotic device, heel cup, or heel cradle for extra support. A heel cup or heel cradle elevates the heel and hereby reduces stress and pressure on the achilles tendon. The device should be made with light-weight, shock absorbing materials.
If the problem persists, consult your foot doctor.
Haglund’s correction and achilles repair 2M
Treatment of arch pain is easy.
Avoid high heels if possible.
Choose footwear with a reasonable soft heel, shock absorbing soles and removable foot insoles.
When the arch pain is due to flat feet, an orthotic usually with a medial arch support is prescribed.
If the problem persists, consult your foot doctor.

Conservative treatment of the arthritic foot includes using proper footwear, orthotics, and/or forefoot supports.Arthritic footwear should have a high, wide area for the toes.Insoles should be flexible and removable.Rocker Soles facilitate walking and reduce stress and pain at the ball-of-the-foot. Arthritic footwear should also allow swelling of the foot.Recommended orthotics are the ones that provide comfort, support and extra cushioning .They reduce pressure and hereby provide comfort and support for the foot.Forefoot supports such as gel toe caps, gel toe shields, gel toe straighteners sometimes help in relieving the pain.
If the problem persists, consult your foot doctor.
Big toe arthrodesis Bilateral 2M
Ankle arthrodesis 8M
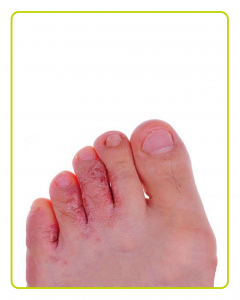
Daily washing of the feet with soap and water followed by thorough drying, especially between the toes helps in preventing Athlete’s Foot.
Wearing dry, wide, airy shoes and socks, not borrowing footwear from others, avoiding tight shoes and using foot powder all help to keep the feet dry and avoid this fungal infection.
When using public showers or pool areas it is a good idea to wear protective slippers.
If an infection has occurred, it is important to see a doctor as if left untreated, fungal infections can become difficult to treat.
Treatment includes antifungal medications, either topical or oral, and proper foot hygiene.
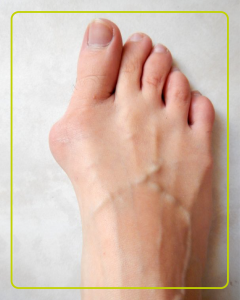
Primary treatment of this condition is to wear shoes that can accommodate the deformity. Shoes designed with a wide toe box are recommended. Orthotics might also be recommended in the case of flat feet. Lastly, surgery is usually the definitive option to correct the deformity.
If the problem persists, consult your foot doctor.
Flatfoot and Hammertoe correction
 Although there is no cure for CMT at the present time, there are many therapies that can greatly improve life and function for CMT patients.
Although there is no cure for CMT at the present time, there are many therapies that can greatly improve life and function for CMT patients.
- Physical therapy can maintain what movement, muscle strength and flexibility they have.
- Many people benefit from occupational therapy which helps people accomplish the tasks of daily living with the use of assistive devices.
- Bracing is another non-invasive form of correcting problems caused by CMT. Often gait abnormalities can be corrected by the use of either hinged or unhinged, braces called AFOs (ankle-foot orthoses). These braces help control foot drop and ankle instability and often provide a better sense of balance for patients.
- Appropriate footwear is important for people with CMT, but they often have difficulty finding well-fitting shoes because of their high arched feet and hammered toes. Falls can generally be avoided by watching where one walks and by wearing appropriate footwear.
- It is important for CMT patients to control their weight. Not only does extra weight make physical activity more difficult, but it also increases the stress on already compromised joints and muscles.
- Patients should try to maintain as much strength and flexibility as possible. Generally, patients should consult a physical therapist or physician before beginning an exercise program, and avoid strenuous activity and overwork. Moderate activity and physical exercise can be beneficial, but patients must be conscious of their physical limitations.
- Finally, stress management is important in maintaining a healthy body.
Any disabling condition can affect the way people think and feel about themselves, but having a chronic illness like CMT, which is often unseen, places stress on individuals and often causes depression. People with CMT can suffer from low self-esteem and relationships with others can be affected.
If the problem persists, consult your doctor.
Changing the type of footwear worn is a very important step in the treatment of claw toes. When choosing a shoe, make sure the toe box (toe area) is high and broad, and can accommodate the claw toes. A shoe with a high, broad toe box will provide enough room in the forefoot area so that there is less friction against the toes. Other conservative treatments include using forefoot products designed to relieve claw toes, such as toe crests and hammer toe splints. These devices will help hold down the claw toe and provide relief to the forefoot. Gel toe shields and gel toe caps are also recommended to eliminate friction between the shoe and the toe, while providing comfort and lubrication. As a final resort, surgery can be performed to correct the deformity.
If the problem persists, consult your foot doctor.
Flatfoot and Hammertoe correction
Footwear and orthotics play an important role in diabetic footcare. Orthotics designed with Plastazote foam; Diabetic footwear should also provide the following protective benefits:
- High, wide toe box (high and wide space in the toe area)
- Removable insoles for fitting flexibility and the option to insert orthotics if necessary.
- Rocker Soles designed to reduce pressure in the areas of the foot most susceptible to pain, most notably the ball-of-the-foot.
- Firm Heel Counters for support and stability.
If you are a diabetic, you should be particularly alert to any problems you may be having with your feet. It is very important for diabetics with neuropathy to take necessary precautions to prevent injury and keep their feet healthy. If you have diabetes and are experiencing a foot problem, immediately consult your foot doctor.
FOOTCARE & DIABETES
Proper footcare is especially critical for diabetics because they are prone to foot problems such as:
- Loss of feeling in their feet
- Changes in the shape of their feet
- Foot ulcers or sores that do not heal
Simple daily footcare can prevent serious problems. The following simple everyday steps will help prevent serious complications from diabetes:
- Take Care of Your Diabetes Make healthy lifestyle choices to keep your blood sugar close to normal. Work with your health care team to create a diabetes plan that fits your lifestyle characteristics.
- Check Your Feet Every Day You may have foot problems that you may not be aware of. Check your feet for cuts, sores, red spots, swelling, or infected toenails. Checking your feet should become part of your daily routine. If you have trouble bending over to see your feet, use a plastic mirror to help. You can also ask a family member to help you. Important Reminder: Be sure to call your doctor immediately if a cut, sore, blister, or bruise on your foot does not heal after one day.
- Wash Your Feet Every Day Wash your feet in warm, NOT HOT, water. Do not soak your feet because your skin will get dry. Before bathing or showering, test the water to make sure it is not too hot. You should use a thermometer or your elbow. Dry your feet well. Be sure to dry between your toes. Use talcum powder to keep the skin dry between the toes.
- Keep the Skin Soft and Smooth Rub a thin coat of skin lotion or cream on the tops and bottoms of the feet. Do not put lotion between your toes, because this might cause infection.
- Wear Shoes and Socks at All Times Wear shoes and socks at all times. Do not walk barefoot, not even indoors. It is extremely easy to step on something and hurt your feet. Always wear seamless socks, stockings, and nylons with your shoes to help avoid the possibility of blisters and sores developing. Be sure to choose seamless socks that are made of materials that wick moisture away from your feet and absorb shock and shear. Socks made of these materials help keep your feet dry. Always check the insides of your shoes before putting them on. Make sure the lining is smooth and there are no foreign objects in the shoe, such as pebbles. Wear shoes that fit well and protect your feet.
- Protect Your Feet from Hot and Cold Always wear shoes at the beach or on hot pavement. Put sunscreen on the tops of your feet for protection from the sun. Keep your feet away from radiators or open fires. DO NOT use hot water bottle or heating pads on your feet. If your feet are cold, wear seamless socks at night. Lined boots are good to keep your feet warm in the winter. Choose socks carefully. DO NOT wear socks with seams or bumpy areas. Choose padded socks to protect your feet and make walking more comfortable. In cold weather, check your feet often to keep your feet warm avoid frostbite.
- Keep the Blood Flowing to Your Feet Put your feet up when you are sitting. Wiggle your toes for 5 minutes, 2 or 3 times a day. Move your ankles up and down and in and out to improve blood flow in your feet and legs.DO NOT cross your legs for long periods of time.
DO NOT wear tight socks, elastic, or rubber bands, or garters around your legs.
DO NOT wear restrictive footwear or foot products. Foot products that can cut off circulation to the feet, such as products with elastic, should not be worn by diabetics.
DO NOT smoke. Smoking reduces blood flow to your feet. If you have high blood pressure or high cholesterol, work with your health care team to lower it. - Be More Active Ask your doctor to plan an exercise program that is right for you. Walking, dancing, swimming, and bicycling are good forms of exercise that are easy on the feet. Avoid all activities that are hard on the feet, such as running and jumping. Always include a short warm-up or cool-down period. Wear protective walking or athletic shoes that fit well and offer good support.
- Communicate with Your Doctor Ask your doctor to check the sense of feeling and pulses in your feet at least once a year. Ask your doctor to tell you immediately if you have serious foot problems. Ask your doctor for proper footcare tips and for the name of your local podiatrist.
If the problem persists, consult your foot doctor.
During symptom-free periods, these dietary guidelines may help protect against future gout attacks:
- Keep your fluid intake high. Stay well-hydrated, including plenty of water.
- Limit your intake of meat, fish and poultry. A small amount may be tolerable, but pay close attention to what types, and how much, seem to cause problems for you.
- Maintain a desirable body weight. Choose portions that allow you to maintain a healthy weight. Losing weight may decrease uric acid levels in your body. But avoid fasting or rapid weight loss, since doing so may temporarily raise uric acid levels.
- Limit or avoid, alcohol especially beer. Talk with your doctor about whether any amount or type of alcohol is safe for you.
- Nonsteroidal anti-inflammatory drugs (NSAIDs). NSAIDs include over-the-counter options such as ibuprofen and naproxen sodium, as well as more-powerful prescription NSAIDs such as indomethacin or celecoxib.
After an acute gout attack resolves, your doctor may prescribe other medications that can control gout pain and symptoms daily dose of colchicine to prevent future attacks.
- Corticosteroid medications, such as the drug prednisone, may control gout inflammation and pain. Corticosteroids may be administered in pill form, or they can be injected into your joint.
Corticosteroids are generally reserved for people who can’t take either NSAIDs or colchicine. Side effects of corticosteroids may include mood changes, increased blood sugar levels and elevated blood pressure.
If you experience several gout attacks each year or if your gout attacks are less frequent but particularly painful, your doctor may recommend medication to reduce your risk of gout-related complications.
If you need further assistance, see your foot doctor.
Big toe Pain
Heel Pain / Plantar Fascitis
Heel Pain and injection
Heel Pain / Plantar Fascitis
TREATMENT AND PREVENTION
Footwear is a very important step in the treatment of hammer toes. When choosing a shoe, make sure the toe box (toe area) is high and broad, and can accommodate the hammer toes. A shoe with a high, broad toe box will provide enough room in the forefoot area so that there is less friction against the toes. Other conservative treatments include using forefoot products designed to relieve hammer toes, such as hammer toe crests and hammer toe splints. These devices will help hold down the hammer toe and provide relief to the forefoot. Gel toe shields and gel toe caps are also recommended to eliminate friction between the shoe and the toe, while providing comfort and lubrication. Surgery can be performed to correct the deformity.
If the problem persists, consult your foot doctor.
Flatfoot and Hammertoe correction
Conservative treatment of mallet toes begins with accommodating the deformity. Shoes with a high and broad toe box (toe area) are recommended for people suffering from forefoot deformities such as mallet toes. This prevents further irritation in the toe area from developing. Other conservative treatment includes forefoot supports such as gel toe caps, gel toe shields and toe crests. Gel forefoot supports provide immediate comfort and relief from common forefoot disorders without drying the skin. Debridement of the corns that may occur due to the deformity, can help temporarily.
If the problem persists, consult your foot doctor.
If the problem persists, consult your foot doctor.
Heel Pain / Plantar Fascitis
Heel Pain and injection
Heel Pain / Plantar Fascitis
Treatment of heel spurs is determining what is causing the excessive stretching of the plantar fascia. If it is due to over-pronation (flat feet), an orthotic with rearfoot posting and longitudinal arch support is an effective device to reduce the over-pronation. Other methods include stretching exercises, losing weight, wearing shoes that have a cushioned heel that absorbs shock, and elevating the heel with the use of a heel cradle, heel cup, or orthotic.
If the problem persists, consult your foot doctor.
Heel Pain / Plantar Fascitis
Heel Pain and injection
Heel Pain / Plantar Fascitis
Conservative treatment of mallet toes begins with accommodating the deformity. Shoes with a high and broad toe box (toe area) are recommended for people suffering from forefoot deformities such as mallet toes. This prevents further irritation in the toe area from developing. Other conservative treatment includes forefoot supports such as gel toe caps, gel toe shields and toe crests. Gel forefoot supports provide immediate comfort and relief from common forefoot disorders without drying the skin. Debridement of the corns that may occur due to the deformity, can help temporarily.
If the problem persists, consult your foot doctor.
Flatfoot and Hammertoe correction
The first step in treating metatarsalgia is to determine the cause of the pain. If improper fitting footwear is the cause of the pain, the footwear must be changed. Footwear designed with a high, wide toe box (toe area) and a rocker sole is ideal for treating metatarsalgia. The high, wide toe box allows the foot to spread out while the rocker sole reduces stress on the ball-of-the-foot. Unloading pressure to the ball-of-the-foot can be accomplished with a variety of footcare products. Orthotics designed to relieve ball-of-foot pain usually feature a metatarsal pad. The orthotic is constructed with the pad placed behind the ball-of-the-foot to relieve pressure and redistribute weight from the painful area to more tolerant areas. Other products often recommended include gel metatarsal cushions and metatarsal bandages. When these products are used with proper footwear, you should experience significant relief.
Flatfoot and Hammertoe correction
The first step is to select proper footwear. Footwear with a high and wide toe box (toe area) is ideal. The next step is to use an orthotic designed with a metatarsal pad that is located below the metatarsal to unload pressure. Cortisone injections are very useful as well. Surgery for this condition, could be used as a last resort.
If problem persists, consult your foot doctor.
Treatment of Morton’s Toe starts with selecting proper footwear. Footwear with a high and wide toe box (toe area) is ideal for treating this condition. It probably better to buy footwear a half size to a size larger to accommodate the longer second toe. Sometimes, orthotics that include arch support, and a metatarsal pad are often recommended when treating this condition.
If problem persists, consult a foot doctor.
Flatfoot and Hammertoe correction
The most successful way to prevent diabetic neuropathy from occurring is to control the diabetes. It is important to maintain blood sugars at normal levels and maintain normal blood pressure. In addition to this, it is important to:
Stop smoking
Have regular physical exams
Have regular blood and urine tests
Exercise regularly, according to your doctor’s recommendation
If alcohol is used then you must limit the amount of alcohol you drink.
It is important for diabetics to treat their feet properly to avoid any future problems. Footwear and foot orthotics play an important role in diabetic footcare. Footwear that fits poorly can cause irritation and injury. Orthotics especially those designed with Plastazote®, are also frequently recommended. Diabetic footwear generally should be: High, with wide toe box (high and wide space in the toe area) Removable insoles for fitting flexibility and the option to insert orthotics if necessary Rocker soles, designed to reduce pressure in the areas of the foot most susceptible to pain, most notably the heel and the ball-of-the-foot. Firm Heel Counters for extra and support and stability. It is important for diabetics with neuropathy to take the necessary precautions to prevent injury and keep their feet healthy.
If you have diabetes and are experiencing a foot problem, immediately consult with your foot doctor.
Diabetic Foot
Diabetic Foot cause :
Diabetic foot / Charcot foot :
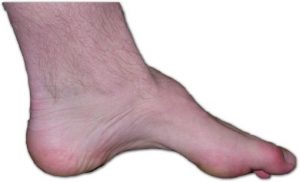
Over-Pronation can be treated conservatively (non-surgical treatments) with custom made orthotics. These orthotics should be designed with appropriate arch support and medial hind foot post to prevent the over-pronation. Footwear with a firm heel counter is often recommended for extra support and stability.
If the problem persists, consult your foot doctor.
Because of the progressive nature of PTTD, early treatment is advised. If treated early enough, your symptoms may resolve without the need for surgery, and progression of your condition can be arrested.
In contrast, untreated PTTD could leave you with an extremely flat foot, painful arthritis in the foot and ankle and increasing limitations on walking, running or other activities.
In many cases of PTTD, treatment can begin with nonsurgical approaches that may include:
- Orthotic devices or bracing. To give your arch the support it needs, your foot and ankle surgeon may provide you with an ankle brace or a custom orthotic device that fits into the shoe.
- Immobilization. Sometimes a short-leg cast or boot is worn to immobilize the foot and allow the tendon to heal, or you may need to completely avoid all weightbearing for a while.
- Physical therapy. Ultrasound therapy and exercises may help rehabilitate the tendon and muscle following immobilization.
- Medications. Nonsteroidal anti-inflammatory drugs (NSAIDs), such as ibuprofen, help reduce the pain and inflammation.
- Shoe modifications. Your foot and ankle surgeon may advise changes to your shoes and may provide special inserts designed to improve arch support.
When Is Surgery Needed?
In cases of PTTD that have progressed substantially or have failed to improve with nonsurgical treatment, surgery may be required. For some advanced cases, surgery may be the only option. Your foot and ankle surgeon will determine the best approach for you.
Make hyperlink
Conservative treatment (non-surgical treatment) of overlapping toes begins with accommodating the disorder. Shoes with a high, broad toe box (toe area) are recommended for people suffering from overlapping toes. Forefoot supports such as gel toe straighteners, gel toe caps and toe combs are often recommended to keep overlapping toes apart. These effective devices are designed to reduce friction to help relieve the discomfort.
If problem persists, consult your foot doctor.
Flatfoot and Hammertoe correction
Obviously determining what is causing the excessive stretching of the plantar fascia is the most important factor. When the cause is over-pronation (flat feet), an orthotic with longitudinal arch support is an effective device. If you have usually high arches, heel cushions, shock absorbers and wearing proper footwear will accommodate and comfort the foot a little. Other common treatments include stretching exercises, plantar fasciitis night splints, wearing shoes that have a cushioned heel to absorb shock, and elevating the heel with the use of a heel cradle or heel cup. Generally, you can reduce the strain and stress on the plantar fascia by following these simple instructions: Avoid running on hard or uneven ground, lose any excess weight, and wear shoes and orthotics that support your arch to prevent over-stretching of the plantar fascia.
If problem persists, consult your foot doctor.
Heel Pain / Plantar Fascitis
Heel Pain and injection
Heel Pain / Plantar Fascitis
There are effective ways to treat both over-pronation and edema during pregnancy. Over-Pronation can be treated conservatively with “ready-made” orthotics. These orthotics should be designed with appropriate arch support and medial rearfoot posting to correct the over-pronation. Proper fitting footwear is also very important in treating over-pronation. Choose comfortable footwear that provides extra support and shock absorption. It is important to treat over-pronation for pain relief but also to prevent other foot conditions from developing such as Plantar Fasciitis, Heel Spurs, Metatarsalgia, Post-Tib Tendonitis and/or Bunions. Edema in the feet can be minimized by the following methods: Elevate your feet as often as possible. If you have to sit for long periods of time, place a small stool by your feet to elevate them. Wear proper fitting footwear. Footwear that is too narrow or short will constrict circulation. Have your feet measured several times throughout your pregnancy. They will probably change sizes. Wear seamless socks that do not constrict circulation. If you are driving for a long period of time, take regular breaks to stretch your legs to promote circulation. Exercise regularly to promote overall health; walking is the best exercise. Drink plenty of water to keep the body hydrated. This helps the body retain less fluid. Eat a well-balanced diet and avoid foods high in salt that can cause water retention. Swelling is normally similar in both feet. If swelling is not symmetrical in both feet, this may be a sign of a vascular problem and a doctor should be contacted immediately.
If any problems persist, consult your doctor.
Treatment is almost always conservative. Minor cases call for a strict period of rest, along with the use of a modified shoe or a shoe pad to reduce pressure on the affected area. This may be accomplished by placing a metatarsal pad that redistributes the pressure of weight bearing to other parts of the forefoot. In addition, the big toe may be bound with tape or athletic strapping to immobilize the joint as much as possible and allow for healing to occur. It is recommended to decrease or stop activity for awhile. This will give your sesamoids time to heal. You should apply ice to the area for 10 to 15 minutes after exercise, or after any activity that aggravates the area. As with icing, anti-inflammatories will help to decrease inflammation so healing can begin. While the injury is healing, women should wear flat shoes on a daily basis.
If home remedies do not work, see your doctor for a correct diagnosis.
Preventing shin splints should be by stretching and strengthening the leg muscles, wearing footwear with good shock absorption, and avoid running on hard surfaces or excessive running or jumping on the ball-of-the-foot. Insoles or orthotics that offer arch support for over-pronation or cavus feet are also important. It is also necessary to temporarily avoid the exercise that is causing the problem until pain subsides. Icing the area immediately after running or other exercise can also be effective, along with stretching before and after training. It is important not to try to train through the pain of shin splints. Runners should decrease their normal running distance for about a week and avoid hills or hard surfaces.
If the problem persists, consult your foot doctor.
How is the pain treated?
Because feet support all our body weight, a simple injury could become a more severe one if it is neglected. Kindly see your doctor as soon as you can.
Treatment depends on the underlying cause of the condition. Thus treatment might include items like :
- physical therapy, which can help in problems such as peripheral neuropathy, extensor tendonitis, and damage to the peroneal nerve
- a cast or walking boot for injuries such as broken bones or fractures
- NSAIDs or other anti-inflammatory drugs, which can help reduce inflammation, including inflammation.
Generally for mild cases of foot pain, you should rest and avoid bearing weight on the foot as much as possible. Apply ice to the painful area for twenty minutes at a time, but no more, maybe three times a day. If you do have to walk, wear supportive, well-fitting shoes that aren’t too tight.
Nonsurgical Treatment
Treatment of ankle fractures depends on the type and severity of the injury. At first, the foot and ankle surgeon will want you to follow the RICE protocol:
- Rest: Stay off the injured ankle. Walking may cause further injury.
- Ice: Apply an ice pack to the injured area, placing a thin towel between the ice and the skin. Use ice for 20 minutes and then wait at least 40 minutes before icing again.
- Compression: An elastic wrap should be used to control swelling.
- Elevation: The ankle should be raised slightly above the level of your heart to reduce swelling.
Additional treatment options include:
- Immobilization. Certain fractures are treated by protecting and restricting the ankle and foot in a cast or splint. This allows the bone to heal.
- Prescription medications. To help relieve the pain, the surgeon may prescribe pain medications or anti-inflammatory drugs.
When Is Surgery Needed?
For some ankle fractures, surgery is needed to repair the fracture and other soft tissue-related injuries, if present. The foot and ankle surgeon will select the procedure that is appropriate for your injury.
Follow-Up Care
It is important to follow your surgeon’s instructions after treatment. Failure to do so can lead to infection, deformity, arthritis and chronic pain.
Nonsurgical Treatment
Treatment for chronic ankle instability is based on the results of the examination and tests, as well as on the patient’s level of activity. Nonsurgical treatment may include:
- Physical therapy. Physical therapy involves various treatments and exercises to strengthen the ankle, improve balance and range of motion and retrain your muscles. As you progress through rehabilitation, you may also receive training that relates specifically to your activities or sport.
- Bracing. Some patients wear an ankle brace to gain support for the ankle and keep the ankle from turning. Bracing also helps prevent additional ankle sprains.
- Medications. Nonsteroidal anti-inflammatory drugs (NSAIDs), such as ibuprofen, may be prescribed to reduce pain and inflammation.
When Is Surgery Needed?
In some cases, the foot and ankle surgeon will recommend surgery based on the degree of instability or lack of response to nonsurgical approaches. Surgery usually involves repair or reconstruction of the damaged ligament(s). The surgeon will select the surgical procedure best suited for your case based on the severity of the instability and your activity level. The length of the recovery period will vary, depending on the procedure or procedures performed.
Chronic ankle instability repair 2M
Nonsurgical Treatment
When you have an ankle sprain, rehabilitation is crucial—and it starts the moment your treatment begins. Your foot and ankle surgeon may recommend one or more of the following treatment options:
- Rest. Stay off the injured ankle. Walking may cause further injury.
- Ice. Apply an ice pack to the injured area, placing a thin towel between the ice and the skin. Use ice for 20 minutes and then wait at least 40 minutes before icing again.
- Compression. An elastic wrap may be recommended to control swelling.
- Elevation. The ankle should be raised slightly above the level of your heart to reduce swelling.
- Early physical therapy. Your doctor will start you on a rehabilitation program as soon as possible to promote healing and increase your range of motion. This includes doing prescribed exercises.
- Medications. Nonsteroidal anti-inflammatory drugs (NSAIDs), such as ibuprofen, may be recommended to reduce pain and inflammation. In some cases, prescription pain medications are needed to provide adequate relief.
When Is Surgery Needed?
In more severe cases, surgery may be required to adequately treat an ankle sprain. Surgery often involves repairing the damaged ligament or ligaments. The foot and ankle surgeon will select the surgical procedure best suited for your case based on the type and severity of your injury as well as your activity level.
After surgery, rehabilitation is extremely important. Completing your rehabilitation program is crucial to a successful outcome. Be sure to continue to see your foot and ankle surgeon during this period to ensure that your ankle heals properly and function is restored.
Chronic ankle instability repair 2M:
Ankle Scope bilateral 2and3M
Nonsurgical treatment of Haglund’s deformity is aimed at reducing the inflammation of the bursa. While these approaches can resolve the pain and inflammation, they will not shrink the bony protrusion. Nonsurgical treatment can include one or more of the following:
- Medication. Oral nonsteroidal anti-inflammatory drugs (NSAIDs), such as ibuprofen, may be recommended to reduce the pain and inflammation. Ice. To reduce swelling, apply an ice pack to the inflamed area, placing a thin towel between the ice and the skin. Use ice for 20 minutes and then wait at least 40 minutes before icing again.
- Exercises. Stretching exercises help relieve tension from the Achilles tendon. These exercises are especially important for the patient who has a tight heel cord.
- Heel lifts. Patients with high arches may find that heel lifts placed inside the shoe decrease the pressure on the heel.
- Heel pads. Pads placed inside the shoe cushion the heel and may help reduce irritation when walking.
- Shoe modification. Backless or soft backed shoes help avoid or minimize irritation.
- Physical therapy. Physical therapy modalities, such as ultrasound, can help to reduce inflammation. Especially so-called Shock wave therapy.
- Orthotic devices. Custom arch supports control the motion in the foot.
- Immobilization. In some cases, casting may be necessary.
When Is Surgery Needed?
If nonsurgical treatment fails to provide adequate pain relief, surgery may be needed. The foot and ankle surgeon will determine the procedure that is best suited to your case. It is important to follow the surgeon’s instructions for postsurgical care.
Prevention
To help prevent a recurrence of Haglund’s deformity:
- wear appropriate shoes; avoid shoes with a rigid heel back
- use arch supports or orthotic devices
- perform stretching exercises to prevent the Achilles tendon from tightening
- avoid running on hard surfaces and running uphill
Haglund’s correction and achilles repair 2M
Nonsurgical Approaches
Relief of the symptoms is often achieved through treatments that can include a combination of the following:
- Rest. It is important to stay off the injured foot to let the inflammation subside.
- Immobilization. A walking boot is often used to restrict ankle motion and to allow the injured tissue to heal.
- Ice. Swelling is decreased by applying a bag of ice covered with a thin towel to the affected area. Do not put ice directly against the skin.
- Oral medication. Nonsteroidal anti-inflammatory drugs (NSAIDs), such as ibuprofen, may be helpful in reducing the pain and inflammation.
- Injections. Sometimes cortisone is injected into the area to reduce the inflammation and pain.
When Is Surgery Needed?
Most patients’ symptoms improve with nonsurgical treatment. However, in some patients, surgery may be required to relieve the symptoms. Surgery typically involves removal of the os trigonum, as this extra bone is not necessary for normal foot function.
Ankle Scope 2 Months
To help relieve symptoms, the surgeon may begin treating osteoarthritis with one or more of the following nonsurgical approaches:
- Oral medications. Nonsteroidal anti-inflammatory drugs (NSAIDs), such as ibuprofen, are often helpful in reducing the inflammation and pain. Occasionally, a prescription for a steroid medication is needed to adequately reduce symptoms.
- Orthotic devices. Custom orthotic devices (shoe inserts) are often prescribed to provide support to improve the foot’s mechanics or cushioning to help minimize pain.
- Bracing. Bracing, which restricts motion and supports the joint, can reduce pain during walking and can help prevent further deformity.
- Immobilization. Protecting the foot from movement by wearing a cast or removable cast-boot may be necessary to allow the inflammation to resolve.
- Steroid injections. In some cases, steroid injections are applied to the affected joint to deliver anti-inflammatory medication.
- Physical therapy. Exercises to strengthen the muscles, especially when osteoarthritis occurs in the ankle, may give the patient greater stability and may help him or her avoid injury that might worsen the condition.
When Is Surgery Needed?
When osteoarthritis has progressed substantially or has failed to improve with nonsurgical treatment, surgery may be recommended. In advanced cases, surgery may be the only option. The goal of surgery is to decrease pain and improve function. The foot and ankle surgeon will consider a number of factors when selecting the procedure best suited to the patient’s condition and lifestyle.
Big toe arthrodesis Bilateral 2M
Ankle arthrodesis 8M
Nonsurgical Treatment
Treatment depends on the type of peroneal tendon injury. Options include:
- Immobilization. A cast or splint may be used to keep the foot and ankle from moving and allow the injury to heal.
- Medications. Oral or injected anti-inflammatory drugs may help relieve pain and inflammation.
- Physical therapy. Ice, heat or ultrasound therapy may be used to reduce swelling and pain. As symptoms improve, exercises can be added to strengthen the muscles and improve range of motion and balance.
- Bracing. The surgeon may provide a brace to use for a short while or during activities requiring repetitive ankle motion. Bracing may also be an option when a patient is not a candidate for surgery.
When Is Surgery Needed?
In some cases, surgery may be needed to repair the tendon or tendons and perhaps the supporting structures of the foot. The foot and ankle surgeon will determine the most appropriate procedure for the patient’s condition and lifestyle. After surgery, physical therapy is an important part of rehabilitation.
Because of the progressive nature of PTTD, early treatment is advised. If treated early enough, your symptoms may resolve without the need for surgery, and progression of your condition can be arrested.
In contrast, untreated PTTD could leave you with an extremely flat foot, painful arthritis in the foot and ankle and increasing limitations on walking, running or other activities.
In many cases of PTTD, treatment can begin with nonsurgical approaches that may include:
- Orthotic devices or bracing. To give your arch the support it needs, your foot and ankle surgeon may provide you with an ankle brace or a custom orthotic device that fits into the shoe.
- Immobilization. Sometimes a short-leg cast or boot is worn to immobilize the foot and allow the tendon to heal, or you may need to completely avoid all weightbearing for a while.
- Physical therapy. Ultrasound therapy and exercises may help rehabilitate the tendon and muscle following immobilization.
- Medications. Nonsteroidal anti-inflammatory drugs (NSAIDs), such as ibuprofen, help reduce the pain and inflammation.
- Shoe modifications. Your foot and ankle surgeon may advise changes to your shoes and may provide special inserts designed to improve arch support.
When Is Surgery Needed?
In cases of PTTD that have progressed substantially or have failed to improve with nonsurgical treatment, surgery may be required. For some advanced cases, surgery may be the only option. Your foot and ankle surgeon will determine the best approach for you.
Treatment depends on the severity of the talar dome lesion. If the lesion is stable (without loose pieces of cartilage or bone), one or more of the following nonsurgical treatment options may be considered:
- Immobilization. Depending on the type of injury, the leg may be placed in a cast or cast boot to protect the talus. During this period of immobilization, non weight-bearing range-of-motion exercises may be recommended.
- Oral medications. Nonsteroidal anti-inflammatory drugs (NSAIDs), such as ibuprofen, may be helpful in reducing the pain and inflammation.
- Physical therapy. Range-of-motion and strengthening exercises are beneficial once the lesion is adequately healed. Physical therapy may also include techniques to reduce pain and swelling.
- Ankle brace. Wearing an ankle brace may help protect the patient from reinjury if the ankle is unstable.
When Is Surgery Needed?
If nonsurgical treatment fails to relieve the symptoms of talar dome lesions, surgery may be necessary. Surgery may involve removal of the loose bone and cartilage fragments within the joint and establishing an environment for healing. A variety of surgical techniques is available to accomplish this. The surgeon will select the best procedure based on the specific case.
Complications of Talar Dome Lesions
Depending on the amount of damage to the cartilage in the ankle joint, arthritis may develop in the joint, resulting in chronic pain, swelling and limited joint motion. Treatment for these complications is best directed by a foot and ankle surgeon and may include one or more of the following:
- Nonsteroidal or steroidal anti-inflammatory medications
- Physical therapy
- Bracing
- Surgical intervention
Ankle OCD treatment 8M
Ankle OCD 2.5M
Ankle OCD 14M
I am text block. Click edit button to change this text. Lorem ipsum dolor sit amet, consectetur adipiscing elit. Ut elit tellus, luctus nec ullamcorper mattis, pulvinar dapibus leo.
A puncture wound must be cleaned properly and monitored throughout the healing process to avoid complications.
Even if you have gone to an emergency room for immediate treatment of your puncture wound, see a foot and ankle surgeon for a thorough cleaning and careful follow-up. The sooner you do this, the better—within 24 hours after injury, if possible.
The surgeon will make sure the wound is properly cleaned and no foreign body remains. He or she may numb the area, thoroughly clean inside and outside the wound, and monitor your progress. In some cases, x-rays may be ordered to determine whether something remains in the wound or if bone damage has occurred. Antibiotics may be prescribed if necessary.
Avoiding Complications
Follow the foot and ankle surgeon’s instructions for care of the wound to prevent complications
- Infection is a common complication of puncture wounds that can lead to serious consequences.
- Sometimes a minor skin infection evolves into a bone or joint infection, so you should look for these signs:
- A minor skin infection may develop two to five days after injury.
- The signs of a minor infection that show up around the wound include soreness, redness and possibly drainage, swelling and warmth. You may also develop a fever.
- If these signs have not improved, or if they reappear in 10 to 14 days, a serious infection in the joint or bone may have developed.
- Other complications that may arise from inadequate treatment of puncture wounds include painful scarring in the area of the wound or a hard cyst where the foreign body has remained in the wound.
- Although the complications of puncture wounds can be quite serious, early and proper treatment can play a crucial role in preventing them.
Puncture Wounds: What You Should Do
- Seek treatment right away.
- Get a tetanus shot if needed (usually every 10 years).
- See a foot and ankle surgeon within 24 hours.
- Follow your doctor’s instructions.
- Keep your dressing dry.
- Keep weight off of the injured foot.
- Finish all your antibiotics (if prescribed).
- Take your temperature regularly. Watch for signs of infection (pain, redness, swelling, fever). Call your doctor if these signs appear.
Nonsurgical Treatment
In many cases, early treatment may prevent or postpone the need for surgery in the future. Treatment for mild or moderate cases of hallux rigidus may include:
- Shoe modifications. Shoes with a large toe box put less pressure on your toe. Stiff or rocker-bottom soles may also be recommended.
- Orthotic devices. Custom orthotic devices may improve foot function.
- Medications. Oral nonsteroidal anti-inflammatory drugs (NSAIDs), such as ibuprofen, may be recommended to reduce pain and inflammation.
- Injection therapy. Injections of corticosteroids may reduce inflammation and pain.
- Physical therapy. Ultrasound therapy or other physical therapy modalities may be undertaken to provide temporary relief.
When Is Surgery Needed?
In some cases, surgery is the only way to eliminate or reduce pain. Several types of surgery are available for treatment of hallux rigidus. In selecting the procedure or combination of procedures for your particular case, the foot and ankle surgeon will take into consideration the extent of your deformity based on the x-ray findings, your age, your activity level and other factors. The length of the recovery period will vary depending on the procedure or procedures performed.
Big toe arthrodesis Bilateral 2M
Consequences of Improper Treatment
Some people say that “the doctor can’t do anything for a broken bone in the foot.” This is usually not true. In fact, if a fractured toe or metatarsal bone is not treated correctly, serious complications may develop. For example:
- A deformity in the bony architecture, which may limit the ability to move the foot or cause difficulty in fitting shoes.
- Arthritis, which may be caused by a fracture in a joint (the juncture where two bones meet), or may be a result of angular deformities that develop when a displaced fracture is severe or has not been properly corrected.
- Chronic pain and deformity.
- Nonunion, or failure to heal, can lead to subsequent surgery or chronic pain.
Treatment of Toe Fractures
Fractures of the toe bones are almost always traumatic fractures. Treatment for traumatic fractures depends on the break itself and may include these options:
- Rest. Sometimes rest is all that is needed to treat a traumatic fracture of the toe.
- Splinting. The toe may be fitted with a splint to keep it in a fixed position.
- Rigid or stiff-soled shoe. Wearing a stiff-soled shoe protects the toe and helps keep it properly positioned. Use of a postoperative shoe or boot is also helpful.
- Buddy taping the fractured toe to another toe is sometimes appropriate, but in other cases, it may be harmful.
- Surgery. If the break is badly displaced or if the joint is affected, surgery may be necessary. Surgery often involves the use of fixation devices, such as pins.
Treatment of Metatarsal Fractures
Breaks in the metatarsal bones may be either stress or traumatic fractures. Certain kinds of fractures of the metatarsal bones present unique challenges.
For example, sometimes a fracture of the first metatarsal bone (behind the big toe) can lead to arthritis. Since the big toe is used so frequently and bears more weight than other toes, arthritis in that area can make it painful to walk, bend or even stand.
Another type of break, called a Jones fracture, occurs at the base of the fifth metatarsal bone (behind the little toe). It is often misdiagnosed as an ankle sprain, and misdiagnosis can have serious consequences since sprains and fractures require different treatments. Your foot and ankle surgeon is an expert in correctly identifying these conditions as well as other problems of the foot.
Treatment of metatarsal fractures depends on the type and extent of the fracture and may include:
- Rest. Sometimes rest is the only treatment needed to promote healing of a stress or traumatic fracture of a metatarsal bone.
- Avoid the offending activity. Because stress fractures result from repetitive stress, it is important to avoid the activity that led to the fracture. Crutches or a wheelchair are sometimes required to offload weight from the foot to give it time to heal.
- Immobilization, casting or rigid shoe. A stiff-soled shoe or other form of immobilization may be used to protect the fractured bone while it is healing. Use of a postoperative shoe or boot is also helpful.
- Surgery. Some traumatic fractures of the metatarsal bones require surgery, especially if the break is badly displaced.
- Follow-up care. Your foot and ankle surgeon will provide instructions for care following surgical or nonsurgical treatment. Physical therapy, exercises and rehabilitation may be included in a schedule for return to normal activities.
Fracture in children
Can my child walk on their feet even if they have a fracture
Can I get fractured without a trauma?
Nonsurgical Treatment
Treatment for tailor’s bunion typically begins with nonsurgical therapies. Your foot and ankle surgeon may select one or more of the following:
- Shoe modifications. Choose shoes that have a wide toe box, and avoid those with pointed toes or high heels.
- Padding. Bunionette pads placed over the area may help reduce pain.
- Oral medications. Nonsteroidal anti-inflammatory drugs (NSAIDs), such as ibuprofen, may help relieve the pain and inflammation.
- Icing. An ice pack may be applied to reduce pain and inflammation. Wrap the pack in a thin towel rather than placing ice directly on your skin.
- Injection therapy. Injections of corticosteroid may be used to treat the inflamed tissue around the joint.
- Orthotic devices. In some cases, custom orthotic devices may be provided by the foot and ankle surgeon.
When Is Surgery Needed?
Surgery is often considered when pain continues despite the above approaches. In selecting the procedure or combination of procedures for your case, the foot and ankle surgeon will take into consideration the extent of your deformity based on the x-ray findings, your age, your activity level and other factors. The length of the recovery period will vary, depending on the procedure or procedures performed.
Nonsurgical Treatment
Nonsurgical treatment of cavus foot may include one or more of the following options:
- Orthotic devices. Custom orthotic devices that fit into the shoe can be beneficial because they provide stability and cushioning to the foot.
- Shoe modifications. High-topped shoes support the ankle, and shoes with heels a little wider on the bottom add stability.
- Bracing. The surgeon may recommend a brace to help keep the foot and ankle stable. Bracing is also useful in managing foot drop.
When Is Surgery Needed?
If nonsurgical treatment fails to adequately relieve pain and improve stability, surgery may be needed to decrease pain, increase stability and compensate for weakness in the foot. The surgeon will choose the best surgical procedure or combination of procedures based on the patient’s individual case. In some cases where an underlying neurologic problem exists, surgery may be needed again in the future due to the progression of the disorder.
The surgeon may select one or more of the following options to treat calcaneal apophysitis:
- Reduce activity. The child needs to reduce or stop any activity that causes pain.
- Support the heel. Temporary shoe inserts or custom orthotic devices may provide support for the heel.
- Medications. Nonsteroidal anti-inflammatory drugs (NSAIDs), such as ibuprofen, help reduce the pain and inflammation.
- Physical therapy. Stretching or physical therapy modalities are sometimes used to promote healing of the inflamed issue.
- Immobilization. In some severe cases of pediatric heel pain, a cast may be used to promote healing while keeping the foot and ankle totally immobile.
Often, heel pain in children returns after it has been treated because the heel bone is still growing. Recurrence of heel pain may be a sign of calcaneal apophysitis or it may indicate a different problem. If your child has a repeat bout of heel pain, be sure to make an appointment with your foot and ankle surgeon.
Can Calcaneal Apophysitis Be Prevented?
The chances of a child developing heel pain can be reduced by:
- Avoiding obesity
- Choosing well-constructed, supportive shoes that are appropriate for the child’s activity
- Avoiding or limiting wearing of cleated athletic shoes
- Avoiding activity beyond a child’s ability.
Treatment
Treatment of calcaneal fractures is dictated by the type of fracture and extent of the injury. The foot and ankle surgeon will discuss with the patient the best treatment—whether surgical or nonsurgical—for the fracture.
For some fractures, nonsurgical treatments may be used. These include:
- Rest, ice, compression and elevation (RICE). Rest (staying off the injured foot) is needed to allow the fracture to heal. Ice reduces swelling and pain; apply a bag of ice covered with a thin towel to the affected area. Compression (wrapping the foot in an elastic bandage or wearing a compression stocking) and elevation (keeping the foot even with or slightly above the heart level) also reduce the swelling.
- Immobilization. Sometimes the foot is placed in a cast or cast boot to keep the fractured bone from moving. Crutches may be needed to avoid weightbearing. For traumatic fractures, treatment often involves surgery to reconstruct the joint, or in severe cases, to fuse the joint. The surgeon will choose the best surgical approach for the patient.
Rehabilitation
Whether the treatment for a calcaneal fracture has been surgical or nonsurgical, physical therapy often plays a key role in regaining strength and restoring function.
Complications of Calcaneal Fractures
Calcaneal fractures can be serious injuries that may produce lifelong problems. Arthritis, stiffness and pain in the joint frequently develop. Sometimes the fractured bone fails to heal in the proper position. Other possible long-term consequences of calcaneal fractures are decreased ankle motion and walking with a limp due to collapse of the heel bone and loss of length in the leg. Patients often require additional surgery and/or long-term or permanent use of a brace or an orthotic device (arch support) to help manage these complications.
Treatment of DVT
If tests indicate a clot is present, the doctor will make a recommendation regarding treatment. Depending on the location of the clot, the patient may need hospitalization. Medical or surgical care will be managed by a team of physicians, which may include a primary care physician, internist, vascular (blood vessel) surgeon or hematologist (blood disease specialist).
Treatment may include:
- Medication. A blood-thinning medication is usually prescribed to help prevent additional clots from forming.
- Compression stockings. Wearing fitted hosiery decreases pain and swelling.
- Surgery. A surgical procedure performed by a vascular specialist may be required.
Complications of DVT
An early and extremely serious complication of DVT is a pulmonary embolism. A pulmonary embolism develops if the clot breaks loose and travels to the lung. Symptoms of a pulmonary embolism include:
- Shortness of breath
- Chest pain
- Coughing up blood
- A feeling of impending doom
A long-term consequence of DVT is damage to the vein from the clot. This damage often results in persistent swelling, pain and discoloration of the leg.
Preventive Measures
For those who have risk factors for DVT, these strategies may reduce the likelihood of developing a blood clot:
- Take blood-thinning medication, if prescribed.
- Reduce risk factors that can be changed. For example, stop smoking and lose excess weight.
- During periods of prolonged immobility, such as on long trips:
- Exercise legs every two to three hours to get the blood flowing back to the heart. Walk up and down the aisle of a plane or train, rotate ankles while sitting and take regular breaks on road trips.
- Stay hydrated by drinking plenty of fluids; avoid alcohol and caffeine.
- Consider wearing compression stockings.
This problem usually responds rather well to physical exercises and physiotherapy. Achilles tendon lengthening exercises are very common and helpful in that respect.
If the problem does not respond to physiotherapy, then lengthening of the tendoachilles or gastrocnemius complex might be required.
Treatment
Treatment options for an Achilles tendon rupture include surgical and nonsurgical approaches. The decision of whether to proceed with surgery or nonsurgical treatment is based on the severity of the rupture and the patient’s health status and activity level.
Nonsurgical Treatment
Nonsurgical treatment, which is generally associated with a higher rate of re-rupture, is selected for minor ruptures, less active patients and those with medical conditions that prevent them from undergoing surgery. Nonsurgical treatment involves use of a cast, walking boot or brace to restrict motion and allow the torn tendon to heal.
Surgery
Surgery offers important potential benefits. Besides decreasing the likelihood of re-rupturing the Achilles tendon, surgery often increases the patient’s push-off strength and improves muscle function and movement of the ankle.
Various surgical techniques are available to repair the rupture. The surgeon will select the procedure best suited to the patient.
Following surgery, the foot and ankle are initially immobilized in a cast or walking boot. The surgeon will determine when the patient can begin weightbearing.
Complications such as incision-healing difficulties, re-rupture of the tendon or nerve pain can arise after surgery.
Physical Therapy
Whether an Achilles tendon rupture is treated surgically or nonsurgically, physical therapy is an important component of the healing process. Physical therapy involves exercises that strengthen the muscles and improve range of motion in the foot and ankle.
Nonsurgical Treatment
Until you are able to see a foot and ankle surgeon, the RICE method of care should be performed:
- Rest: Stay off the injured foot. Walking may cause further injury.
- Ice: Apply an ice pack to the injured area, placing a thin towel between the ice and the skin. Use ice for 20 minutes and then wait at least 40 minutes before icing again.
- Compression: An elastic wrap should be used to control swelling.
- Elevation: The foot should be raised slightly above the level of your heart to reduce swelling.
The foot and ankle surgeon may use one of these nonsurgical options for treatment of a fifth metatarsal fracture:
- Immobilization. Depending on the severity of the injury, the foot is kept immobile with a cast, cast boot or stiff-soled shoe. Crutches may also be needed to avoid placing weight on the injured foot.
- Bone stimulation. A pain-free external device is used to speed the healing of some fractures. Bone stimulation, most commonly used for Jones fractures, may be used as part of the treatment or following an inadequate response to immobilization.
When Is Surgery Needed?
If the injury involves a displaced bone, multiple breaks or has failed to adequately heal, surgery may be required. The foot and ankle surgeon will determine the type of procedure that is best suited to the individual patient.
Nonsurgical Treatment
Many treatment options, often used in combination, are available to treat tarsal tunnel syndrome. These include:
- Rest. Staying off the foot prevents further injury and encourages healing.
- Ice. Apply an ice pack to the affected area, placing a thin towel between the ice and the skin. Use ice for 20 minutes and then wait at least 40 minutes before icing again.
- Oral medications. Nonsteroidal anti-inflammatory drugs (NSAIDs), such as ibuprofen, help reduce the pain and inflammation.
- Immobilization. Restricting movement of the foot by wearing a cast is sometimes necessary to enable the nerve and surrounding tissue to heal.
- Physical therapy. Ultrasound therapy, exercises and other physical therapy modalities may be prescribed to reduce symptoms.
- Injection therapy. Injections of a local anesthetic provide pain relief, and an injected corticosteroid may be useful in treating the inflammation.
- Orthotic devices. Custom shoe inserts may be prescribed to help maintain the arch and limit excessive motion that can cause compression of the nerve.
- Shoes. Supportive shoes may be recommended.
- Bracing. Patients with flatfoot or those with severe symptoms and nerve damage may be fitted with a brace to reduce the amount of pressure on the foot.
When Is Surgery Needed?
Sometimes surgery is the best option for treating tarsal tunnel syndrome. The foot and ankle surgeon will determine if surgery is necessary and will select the appropriate procedure or procedures based on the cause of the condition.
Nonsurgical Treatment
Anyone who has symptoms of a Lisfranc injury should see a foot and ankle surgeon right away. If unable to do so immediately, it is important to stay off the injured foot, keep it elevated (at or slightly above hip level) and apply a bag of ice wrapped in a thin towel to the area every 20 minutes of each waking hour. These steps will help keep the swelling and pain under control.
Treatment by the foot and ankle surgeon may include one or more of the following, depending on the type and severity of the Lisfranc injury:
- Immobilization. Sometimes the foot is placed in a cast to keep it immobile, and crutches are used to avoid putting weight on the injured foot.
- Oral medications. Nonsteroidal anti-inflammatory medications (NSAIDs), such as ibuprofen, help reduce pain and inflammation.
- Ice and elevation. Swelling is reduced by icing the affected area and keeping the foot elevated, as described above.
- Physical therapy. After the swelling and pain have subsided, physical therapy may be prescribed.
When Is Surgery Needed?
Certain types of Lisfranc injuries require surgery. The foot and ankle surgeon will determine the type of procedure that is best suited to the individual patient. Some injuries of this type may require emergency surgery.
Complications of Lisfranc Injuries
Complications can and often arise following Lisfranc injuries. A possible early complication following the injury is compartment syndrome, in which pressure builds up within the tissues of the foot, requiring immediate surgery to prevent tissue damage. A buildup of pressure could damage the nerves, blood vessels and muscles in the foot. Arthritis and problems with foot alignment are very likely to develop. In most cases, arthritis develops several months after a Lisfranc injury, requiring additional treatment.
Nonsurgical Treatment
The goal of nonsurgical treatment of tarsal coalition is to relieve the symptoms and to reduce the motion at the affected joint. One or more of the following options may be used, depending on the severity of the condition and the response to treatment:
- Oral medications. Nonsteroidal anti-inflammatory drugs (NSAIDs), such as ibuprofen, may be helpful in reducing the pain and inflammation.
- Physical therapy. Physical therapy may include massage, range-of-motion exercises and ultrasound therapy.
- Steroid injections. An injection of cortisone into the affected joint reduces the inflammation and pain. Sometimes more than one injection is necessary.
- Orthotic devices. Custom orthotic devices can be beneficial in distributing weight away from the joint, limiting motion at the joint and relieving pain.
- Immobilization. Sometimes the foot is immobilized to give the affected area a rest. The foot is placed in a cast or cast boot, and crutches are used to avoid placing weight on the foot.
- Injection of an anesthetic agent. Injection of an anesthetic into the leg may be used to relax spasms and is often performed prior to immobilization.
When Is Surgery Needed?
If the patient’s symptoms are not adequately relieved with nonsurgical treatment, surgery is an option. The foot and ankle surgeon will determine the best surgical approach based the patient’s age, condition, arthritic changes and activity level.
Nonsurgical Treatment Approaches
The goal of nonsurgical treatment for accessory navicular syndrome is to relieve the symptoms. The following may be used:
- Immobilization. Placing the foot in a cast or removable walking boot allows the affected area to rest and decreases the inflammation.
- Ice. To reduce swelling, a bag of ice covered with a thin towel is applied to the affected area. Do not put ice directly on the skin.
- Medications. Oral nonsteroidal anti-inflammatory drugs (NSAIDs), such as ibuprofen, may be prescribed. In some cases, oral or injected steroid medications may be used in combination with immobilization to reduce pain and inflammation.
- Physical therapy. Physical therapy may be prescribed, including exercises and treatments to strengthen the muscles and decrease inflammation. The exercises may also help prevent recurrence of the symptoms.
- Orthotic devices. Custom orthotic devices that fit into the shoe provide support for the arch and may play a role in preventing future symptoms.
Even after successful treatment, the symptoms of accessory navicular syndrome sometimes reappear. When this happens, nonsurgical approaches are usually repeated.
When Is Surgery Needed?
If nonsurgical treatment fails to relieve the symptoms of accessory navicular syndrome, surgery may be appropriate. Surgery may involve removing the accessory bone, reshaping the area and repairing the posterior tibial tendon to improve its function. This extra bone is not needed for normal foot function.
Nonsurgical Treatment
Treatment includes strategies aimed at relieving the symptoms and conditions associated with equinus. In addition, the patient is treated for the equinus itself through one or more of the following options:
- Night splint. The foot may be placed in a splint at night to keep it in a position that helps reduce tightness of the calf muscle.
- Heel lifts. Placing heel lifts inside the shoes or wearing shoes with a moderate heel takes stress off the Achilles tendon when walking and may reduce symptoms.
- Arch supports or orthotic devices. Custom orthotic devices that fit into the shoe are often prescribed to keep weight distributed properly and to help control muscle/tendon imbalance.
- Physical therapy. To help remedy muscle tightness, exercises that stretch the calf muscle(s) are recommended.|
When Is Surgery Needed?
In some cases, surgery may be needed to correct the cause of equinus if it is related to a tight tendon or a bone blocking the ankle motion. The foot and ankle surgeon will determine the type of procedure that is best suited to the individual patient.